IVF treatments have evolved over the years, offering multiple variations and techniques to suit different fertility challenges and increase the chances of successful pregnancy. Each type is designed to address specific conditions, and the choice of IVF method depends on the couple’s unique fertility issues, medical history, and treatment goals. Here’s an overview of the main types of IVF treatments available today.
1. Conventional IVF
Conventional IVF is the most common form of IVF treatment and involves the following steps:
- Ovarian Stimulation: The woman takes hormone injections to stimulate the ovaries to produce multiple eggs.
- Egg Retrieval: The eggs are retrieved from the ovaries in a minor surgical procedure.
- Fertilization: The eggs are fertilized with sperm in a lab, and the resulting embryos are monitored for several days.
- Embryo Transfer: The best embryo(s) is transferred into the uterus to promote pregnancy.
Conventional IVF is suitable for many types of infertility and is the standard treatment for those without male factor infertility.
2. Intracytoplasmic Sperm Injection (ICSI)
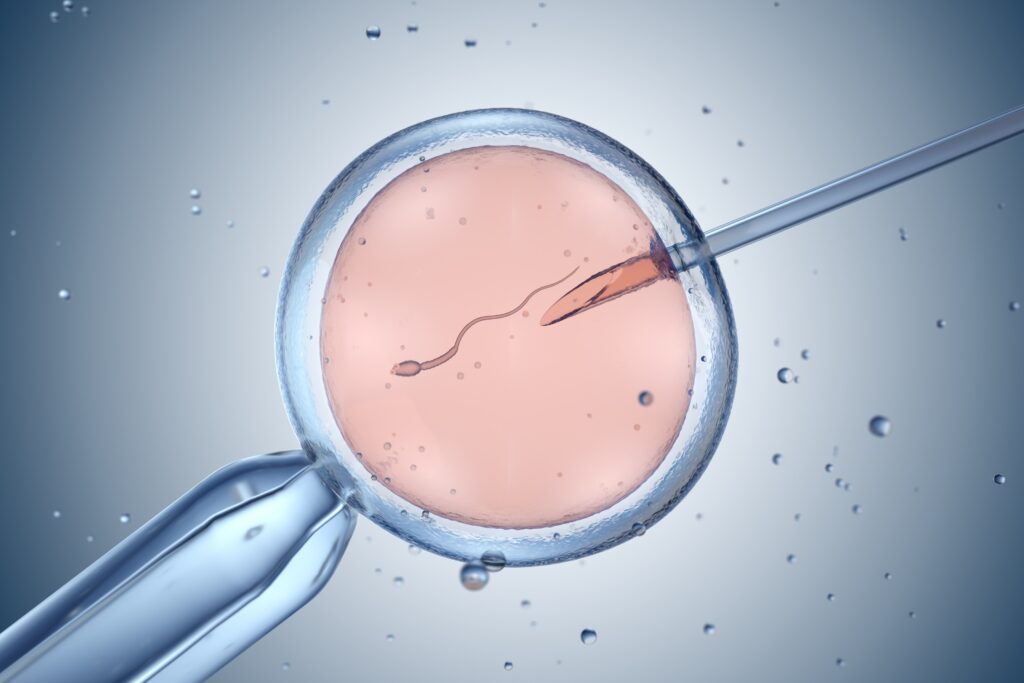
ICSI is a specialized form of IVF primarily used when male infertility issues are present, such as low sperm count or poor motility. Here’s how it works:
- Single Sperm Injection: Instead of mixing eggs with sperm, a single, healthy sperm is injected directly into each egg.
- Embryo Transfer: Once fertilization is achieved, embryos are monitored and transferred like in conventional IVF.
ICSI improves the chances of fertilization in cases where traditional IVF might fail due to sperm-related issues.
3. Natural Cycle IVF
Natural Cycle IVF is a variation that involves minimal or no hormone stimulation. This method is ideal for women who cannot or prefer not to take hormonal medications. Key features include:
- Single Egg Retrieval: Only the naturally produced egg from a woman’s menstrual cycle is retrieved, with no additional hormone stimulation.
- Lower Intervention: Since there’s no ovarian stimulation, this method is less invasive, with fewer side effects.
Natural Cycle IVF may be suitable for women with regular ovulation who prefer a natural approach, though success rates may be lower due to retrieving only one egg per cycle.
4. Mini IVF (Mild Stimulation IVF)
Mini IVF, or minimal stimulation IVF, uses a lower dose of hormones compared to conventional IVF. This option is less intense and may be more comfortable for some women. Key points include:
- Low-Dose Hormonal Stimulation: Hormone levels are adjusted to produce fewer eggs, typically 2-5, rather than a larger batch.
- Reduced Cost and Side Effects: Mini IVF may be less costly than conventional IVF and has a lower risk of side effects like ovarian hyperstimulation syndrome (OHSS).
Mini IVF is often recommended for women with a high risk of OHSS or for those who wish to avoid high hormone doses.
5. Preimplantation Genetic Testing (PGT) with IVF
IVF with preimplantation genetic testing (PGT) is an advanced form of IVF that screens embryos for genetic disorders or chromosomal abnormalities. It involves:
- Genetic Screening: A few cells are biopsied from each embryo before transfer and tested for specific genetic or chromosomal issues.
- Higher Success Rates and Reduced Miscarriage Risk: Selecting only healthy embryos may increase pregnancy success rates and reduce the chances of genetic disorders.
PGT is recommended for couples with a family history of genetic diseases, those with recurrent pregnancy loss, or older women at higher risk of chromosomal abnormalities in their embryos.
6. Frozen Embryo Transfer (FET)
In Frozen Embryo Transfer (FET), previously frozen embryos from an earlier IVF cycle are thawed and transferred into the uterus. This type of IVF is beneficial for:
- Patients with Multiple Embryos: FET allows patients to use embryos from a previous cycle, avoiding the need for repeated egg retrieval.
- Flexible Timing: Patients can plan pregnancy at a later date, which is especially helpful for those undergoing medical treatments or needing a break between cycles.
FET also allows clinics to use advanced embryo screening or genetic testing on the embryos before they are frozen.
7. Donor Egg IVF
Donor Egg IVF is a form of IVF that uses eggs donated by another woman. This is typically an option for women who are unable to produce viable eggs. Here’s what it involves:
- Egg Donation: Donor eggs are fertilized with the male partner’s sperm, creating embryos that are then transferred to the intended mother’s uterus.
- Increased Success Rates: Since donor eggs are often from younger women, the chances of pregnancy can be higher.
This option is ideal for women with diminished ovarian reserve, premature ovarian failure, or other fertility issues preventing them from producing healthy eggs.
9. Assisted Hatching with IVF
Assisted hatching is a technique sometimes used alongside IVF to improve implantation rates. This process involves:
- Thinning the Embryo’s Outer Shell: A small opening is made in the embryo’s outer layer (zona pellucida) to assist the embryo in “hatching” and implanting in the uterus.
- Best for Certain Patients: Assisted hatching is often used for patients with previous failed IVF cycles, older women, or those with embryos that appear to have a thicker outer shell.
Assisted hatching can be helpful for certain fertility challenges, though not all patients will need this procedure.
Conclusion
The different types of IVF treatments offer unique solutions to various fertility challenges. The choice of treatment depends on individual circumstances, such as age, health, infertility cause, and personal preferences. Consulting with a fertility specialist can help determine the best IVF type for your situation and provide a tailored plan that aligns with your reproductive goals.